[Биотехнологии, Здоровье] Glaucoma — how not to go blind: let's talk about the treatment… (перевод)
Автор
Сообщение
news_bot ®
Стаж: 7 лет 11 месяцев
Сообщений: 27286
We know that nobody is immune to glaucoma.
The number of patients with glaucoma worldwide more than 100 million (!) People. Nine out of ten blind people live in developing countries, and two thirds of them could be cured, they begin to be treated on time.
Glaucoma is the second cause of blindness after cataract — up to 20% of all cases of the disease end with it. Some people do not know about the disease. Glaucoma is often detected at stage 2–3 or at the last, 4th stage, when it is often impossible to help a person. In Russia, glaucoma has recently become the first cause of irreversible blindness, overtaking injury and vascular eye disease.
Despite a serious breakthrough in the understanding of many of the problems of glaucoma over the past few years, it must be admitted that so far no effective methods have been proposed to prevent the disease, its early (fairly cheap method!) Identification and treatment methods that are widely available.
The trouble is that the prevention of this disease, we have long ceased. Previously, after forty, all Soviet people were sure to measure eye pressure once a year. In clinics there were professional examination rooms, people with elevated intraocular pressure were referred to an ophthalmologist. And so revealed about half of patients with glaucoma. Now there is nothing like this. Saving patients was the work of the patients themselves (that is, drowning people).

Since the treatment of glaucoma is just as dangerous as caving — you climb into the dark, and when and what falls on your head, science is unknown. But if you don’t fall, you will drown or suffocate yourself — there are options. When you guess where you are, it will be too late. Let me start with a number of rules described below.
Rule number 1
If you have been diagnosed with glaucoma, this disease will accompany you throughout your life. This means that some part of the optic nerve has suffered. Therefore, one cannot say — “I have glaucoma removed” even after surgery. Living with glaucoma is not a sentence, but we must not forget about it.
Rule number 2
This imposes a number of lifelong limitations and requires the regular use of drops — about them below. If you are respectful of your illness, the rate of its progression will slow down significantly.
Rule number 3
Regular lifetime visits to an ophthalmologist are needed to monitor the level of intraocular pressure. Ideally, monthly. Once every 6 months you need to do research to assess the visual fields and tomograms of the optic nerves of both eyes. This is a dynamic control.
Believe me, those patients who did not observe appointments lost sight, refused surgical treatment, disappeared for months and years, and then lamented that vision was irretrievably lost.
Rule number 4
If nothing hurts, do not think that there is no disease and all the dangers are exaggerated. A feature of glaucoma is the absence of symptoms in the early and advanced stages of the disease. The patient himself does not know about the disease until he begins to lose his sight.

In order to notice the disease in time, preventive examination by an ophthalmologist is necessary. You need to pass it once a year, and after 50 years — twice a year.
Rule number 5
Do not look for a “wonderful” pill, “magic” drops or devices that “heal all ailments”, which are so actively offered on the pages of newspapers, on radio and television, on the Internet, telling tips on how to cure glaucoma with folk remedies. This way you will lose that valuable time for treatment and it will be impossible to catch up.
Use evidence-based medicine methods!
What is the treatment for glaucoma currently?
All types of treatment for glaucoma are aimed at normalizing intraocular pressure, improving nutrition in the tissues of the eye and in the optic nerve, as well as stabilizing visual functions.
Conservative treatment of glaucoma
That is, the instillation of various types of drops in a certain mode, and for each eye, it is selected separately.
This therapy is most common in the early stages of glaucoma treatment. It can also be an addition to other types of treatment — laser or surgical.
Some medicinal substances are aimed at reducing the production of intraocular fluid. Others, with the help of special mechanisms, are aimed at improving the outflow of intraocular fluid and thereby lowering the intraocular pressure. Also, there are combined drugs that combine both directions.

Are the drops of glaucoma harmless?
Modern drops of glaucoma are in most cases effective, but not always harmless.
Drops contain the active substance in the form of a solution, as well as a preservative, for example, benzalkonium hydrochloride. It has a negative effect on the eye surface. With prolonged use (we are talking about years), especially if the doctor does not change the drug, and the patient for a long time uses the same medicine, dry eye syndrome may develop (redness, pain, dryness).
Allergic reactions and intolerance of drugs of the general and local character are possible.
In addition, reactions of the body as a whole are possible, for example, interruptions in heart rhythm, lowering of blood pressure, sleep disturbance and dizziness, etc.
A competent doctor from a huge arsenal of drops must choose a suitable one or find a replacement. If this does not work, surgical assistance is needed.
Drug treatment of glaucoma is prescribed by an ophthalmologist only after a complete ophthalmologic examination is entirely individual — how it is written here.
It is very dangerous to self-treat glaucoma — do not use or cancel antiglaucoma drugs yourself, do not violate the mode and frequency of instillation. With these actions, you can cause irreparable harm to your eyes and lose your sight.

And, here's another, in my (and not only) opinion — taufon and emoxipin, so loved by all — are useless with this diagnosis. Glaucoma and cataracts are not treated. The lens and the optic nerve do not reach. «Holy water» and more efficiently.
Laser treatment for glaucoma
1. Patients love the word «laser.» So, only with angle-closure glaucoma, it is 100% effective. In cases of closed and narrow angles, a procedure such as laser iridectomy is the guarantor of prevention of an angle-closure glaucoma attack.
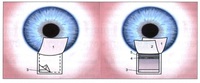
In the case of angle-closure glaucoma (we wrote about it here ), the angle of the anterior chamber, in which the main outflow collector of the Schlemm's canal passes, is blocked by the iris root. By the way, this condition can be periodic, for example, it can manifest itself only when the pupil is dilated (at night, under stress, etc.).
Predisposing factors — farsightedness (“short eye”) + “thick” lens (thickens with age) + front attachment of the lens + small front camera
Then this is what happens:

The fluid accumulates in the back of the chamber, the iris overlaps the outflow channel, the pressure rises, the person experiences pain in the eye, the eye becomes red and there may be a loss of vision if you do not unlock the outflow.
In this case, a hole is made in the iris using a perforator laser — peripheral laser iridectomy (iridotomy). It is also proposed to perform in the case when the angle of the front camera has not yet closed, but there is such a risk. Narrow angles are determined by inspection with a special goniscopic lens.

So schematically looks laser iridectomy and the eye after it under a microscope
And here is a video of the procedure:
Извините, данный ресурс не поддреживается. :(
If the laser fails to perform the opening, surgical iridectomy is performed under operating conditions.
Laser iridectomy is performed using laser systems with different wavelengths: using a single-pulse solid-state neodymium YAG laser or a gas argon laser.
2. Now about laser treatment for open-angle glaucoma. And I remind you that 80% of all cases it is she who is open-angle glaucoma. It's all not so simple. The varieties of laser surgery in the treatment of open-angle glaucoma are laser trabeculoplasty or trabeculo-puncture. The method involves applying point burn applications on a specific part of the trabeculae (the network through which the outflow is taking place).

It is assumed that the pigment that litters the trabeculae is “knocked out”, the fibers shrink and increase the spacing for outflow — they achieve a “popcorn effect”. For this, argon and neodymium laser trabeculoplasty (LTP) (514/532 nm) and diode infrared or micropulse LTP (810 nm) are used.
In fact, such a procedure in itself can further increase the intraocular pressure, if the effect is, then it is very short-lived and unstable. As an independent procedure, it is dangerous, since after it the patients consider themselves to be a “cured” laser and often stop dropping drops and stop visits to the ophthalmologist. And glaucoma is quietly progressing!
Laser procedures such as descemetonogonopuncture (BPH)With the help of these lasers, we often use in addition to microsurgical non-penetrating deep sclerectomy (NSEG), which will be discussed further. Then the shots are applied on the Descemet membrane, and not on the channel — it turns into a «sieve» and further enhances the outflow.
3. And finally, the laser for cyclophotocoagulation. In this case, it doesn't matter what was the cause.
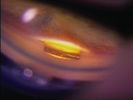
Used in the advanced end stage of the disease. When the eye does not see or hardly sees, it begins to hurt and bother. On the surface of the eyeball or from inside it (using an endoscope combined with a laser) coagulates are applied at a distance of 1.5 — 3 mm from the limbus in the projection area of the processes of the ciliary body, a rather painful procedure.

Outdoor cyclophotocoagulation (DPC)

Schematic representation of endoscopic cyclophotocoagulation.
As a result of coagulation of the secreting ciliary epithelium, which produces intraocular fluid, intraocular pressure decreases. You can use a diode laser (810 nm) and neodymium laser (1064 nm).
Therefore, the conclusion is that not all lasers are equally useful; a laser can eliminate the cause of glaucoma only with angle-closure glaucoma. A modern ophthalmologic clinic should have at least three types of laser systems for the treatment of various glaucoma variants.
Surgical treatment of glaucoma
Surgical treatment of glaucoma is aimed at creating an alternative system of intraocular fluid outflow, or at normalizing the circulation of intraocular fluid or reducing its production. This allows you to save the patient from drops or reduce dependence on them. The question of the surgical treatment of glaucoma is decided on the basis of the data of the dynamics of glaucoma strictly individually and depends on the form and its stage, the level of intraocular pressure increase, the outflow coefficient, the state of the anterior chamber angle, the visual field, and the general somatic state of the patient.
Types of antiglaucoma operations
1. 1. Non-penetrating (non-fistulatizing) antiglaucoma operations. For example, non-penetrating deep sclerectomy (NSEG);
In the upper part of the limbus, under the upper eyelid, a pocket of about 4 × 5 mm is formed in the middle layers of the sclera, part of the Schlemm's canal with its inner wall is exposed and removed, and the area of the Descemet membrane adjacent to the limbus is capable of filtering intraocular fluid. To extend the “service life” of this operation, drainage is placed in the pocket (it can be from different materials, for example, collagen) — this prevents adhesion of the pocket walls and scarring in the area of operation.
Usually this type of surgery is the primary choice for open-angle glaucoma, because:
- It is as safe as possible, since there are no pressure drops — the eye cavity does not open and the pressure decreases smoothly.
- It can be very convenient to combine, if necessary, to simultaneously perform antiglaucoma surgery and cataract surgery
- There are many drains that enhance and prolong the result of the operation.
- When properly performed by the surgeon, the risks of potential complications are reduced to an unlikely minimum.
- It is performed on an outpatient basis and the rehabilitation period is 1-2 days.

Outpatient microsurgery of glaucoma
2. 2. Penetrating (fistulizing) antiglaucoma operations. For example, trabeculectomy;
In this case, a pocket is also formed in the middle layers of the sclera, part of the Schlemm's canal is removed, the eye is opened and the hole in the iris is surgically performed (the iris coloboma).
The difference with the non-penetrating operation is in the opening of the eyeball — in the case of penetrating surgery, the eye is opened, in the case of non-penetrating surgery, a thin semi-permeable Descemet membrane remains intact, due to which the eye is sealed.

It is used in cases of more developed glaucoma and the need for a second operation. An older type of surgery, with various types of drainage that prevent scarring.

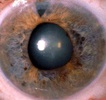
The patient's eye after surgery.
Penetrating operations are more dangerous, as they can cause postoperative hypotension (long-term persistent pressure reduction), intraocular inflammation and hemorrhage, the appearance of cataracts, but have a longer service life.
Types of drainage
There are a great variety of drainage types — they differ in the type of material: hydrogel, collagen, metal and plastic.
The shape can be rectangular, oval, square and triangular.
They can be solid or porous, be a tube or a “nail.”
There are so-called valve drains (Ahmed or Malteno) — this is a system of tubes with a plastic “pocket” that provide communication between the anterior chamber of the eye and the space between the eye shells. outflow. Inside the tubes are valves that are able to regulate the flow of intraocular fluid.
Which is better? There is no ideal, everything is very individual. Everything as always depends on the experience and common sense of the surgeon.
Ahmed’s valve looks like this schematically:

And so — «live»:
«Nail» -mini shunt, made of steel:

Drainage of gold is rather expensive and very fragile:
3. Operations that normalize the circulation of aqueous humor. For example, iridectomy (with closed anterior chamber angle).

In case the angle of the anterior chamber is blocked by the iris root, by opening the anterior chamber of the eye we can make a hole in the iris and restore the flow of fluid from the posterior chamber to the anterior chamber of the eye. Microsurgical techniques have made iridectomy less traumatic and practically safe operation.
These operations include iridocycloretraction and others. This type of operation is less predictable in terms of efficiency, is associated with complications such as hemorrhages into the eye cavity, the appearance and rapid maturation of cataracts, and chronic inflammatory process.
4. Operations that reduce the production of aqueous humor. For example, cyclic cryoagulation.
Cyclotriocoagulation is carried out at the terminal stage of glaucoma, as well as in the case of ineffectiveness of trabeculectomy or other similar operations. The zone that produces intraocular fluid can not only be destroyed by a laser — it can be “frozen”. During cyclocryocoagulation using a special cryoprobe on the surface of the sclera cause burns in the projection of the ciliary body, which are arranged in a circle. In the area of burns of a cryoprobe, cells of the ciliary body atrophy due to the influence of low temperatures. As a result, the amount of watery moisture produced is reduced. Exposure 1-2 minutes, 6-8 objects, temperature -130 ° — 150 ° C.

In short, a burn or frostbite helps to reduce pressure as an attempt to save the eye as an organ that, unfortunately, does not see.
5. Canaloplasty — plastic of the Schlemm’s canal.
The canal of Schlemm (named after the German anatomist Friedrich Schlemm in the 9th-9th century) is the main transport collector draining aqueous humor (speed of about 2-3 microliters per minute) from the anterior chamber of the eye through numerous grids veins of the skull.
This is a vessel that goes around the junction of the cornea and the iris in the thickness of the sclera in the corner of the anterior chamber.
The channel in its structure resembles a lymphatic vessel. The inner part of the canal, which comes into close contact with the watery moisture, is covered with a microporous (trabecular) network. This site has the greatest resistance to the outflow of aqueous humor. If the canal trunk or its mesh structure is blocked, glaucoma will develop.
It occurs in atherosclerosis, diabetes, injury or infection of the eye.
This is how Schlemm's channel looks in full face and profile:

ОThe operations on the canal include expanding it with various probes and cans, holding special threads “in a circle”, dissection (ab interno trabeculectomy) and, finally, simply filling it with viscous fluids (for example, vysokanalostomy).
It looks like canaloplasty thread:

However, such operations at best give a very short-lived effect due to scarring and recurrent blockage. But scientific research in this direction is constantly being conducted.
When does glaucoma need surgery?
Surgical treatment is an alternative to drug therapy in the initial stage and the only possible way to preserve vision and stabilize the disease in the advanced and advanced stages. Usually, a surgical operation for glaucoma is prescribed with a decrease or absence of the effectiveness of treatment with drugs and the loss of the effect of laser surgery for glaucoma. The period of rehabilitation after operations for glaucoma is usually minimal, there are some small limitations in the postoperative period, but the patient can start work after a few days.
What is acute glaucoma?
This is a very dangerous critical condition resulting from a sharp increase in intraocular pressure.
An acute attack of glaucoma usually begins suddenly. Usually, with the appearance of pain in the eyeball, and the corresponding half of the head, especially often in the occipital region, it may be accompanied by nausea, often vomiting and general weakness. An acute attack of glaucoma can be confused with a migraine, hypertensive crisis, and even food poisoning; pains can spread to the area of the heart and abdomen that are similar to those in cardiovascular diseases.
An acute attack of glaucoma appears for no apparent reason against the background of complete health — suddenly there are pains in the eye and in the head, the eye becomes red and watery, the vision decreases, there may appear “rainbow rings” around the sources of light and fogging. The intraocular pressure may increase to 60–80 mm Hg. Art., stops almost or completely outflow of intraocular fluid from the eye. To the touch such an eye becomes as dense as a stone.
Errors in the diagnosis are expensive, as the patient begins to be treated for another condition, and the necessary emergency care in case of an acute attack does not have glaucoma. If, within 1-2 days after the onset of an attack, the intraocular pressure is not reduced with the help of drugs, laser or surgically, the optic nerve dies and the loss of vision becomes irreversible.

Other posts on the topic
- Glaucoma — not heard of it? Meet the serial silent view killer
- Cataract: it is waiting for you personally (if you live, of course)
===========
Источник:
habr.com
===========
===========
Автор оригинала: Tatiana Shilova
===========Похожие новости:
- [Биотехнологии, Здоровье] Glaucoma — not heard of it? Meet the serial silent view killer (перевод)
- [Здоровье] Как сбросить более 20 кг за несколько месяцев и не набрать их обратно
- [Здоровье] Нейробиология зависимости
- [Accessibility, Гаджеты, Здоровье, Научно-популярное] Как выбрать дисплей Брайля? Незрячие эксперты поделились опытом работы с тифлотехникой
- [Искусственный интеллект, Накопители, Разработка мобильных приложений, Здоровье, Софт] VeChain Has Introduced Blockchain-Based Healthcare Data Management Platform At Cyprus Hospital
- [Биотехнологии, Здоровье] Presbyopia: «menopause» of the eyes in men and women (перевод)
- [Биотехнологии, Здоровье, Лазеры] Presbyopia: «menopause» of the eyes in men and women (перевод)
- [Здоровье, Мозг] Сон и продолжительность жизни. Пандемия недосыпа
- [Исследования и прогнозы в IT, Научно-популярное, Здоровье] COVID-19: Модель параметрического предсказания эпидемии
- [Здоровье, Лайфхаки для гиков] Карантин дома. Обеззараживаем воздух УФ-рециркулятором
Теги для поиска: #_biotehnologii (Биотехнологии), #_zdorove (Здоровье), #_glaucoma, #_ophthalmology, #_eye_clinic, #_blog_kompanii_klinika_oftalmologii_doktora_shilovoj (
Блог компании Клиника офтальмологии доктора Шиловой
), #_biotehnologii (
Биотехнологии
), #_zdorove (
Здоровье
)
Вы не можете начинать темы
Вы не можете отвечать на сообщения
Вы не можете редактировать свои сообщения
Вы не можете удалять свои сообщения
Вы не можете голосовать в опросах
Вы не можете прикреплять файлы к сообщениям
Вы не можете скачивать файлы
Текущее время: 14-Янв 22:39
Часовой пояс: UTC + 5
| Автор | Сообщение |
|---|---|
|
news_bot ®
Стаж: 7 лет 11 месяцев |
|
|
We know that nobody is immune to glaucoma. The number of patients with glaucoma worldwide more than 100 million (!) People. Nine out of ten blind people live in developing countries, and two thirds of them could be cured, they begin to be treated on time. Glaucoma is the second cause of blindness after cataract — up to 20% of all cases of the disease end with it. Some people do not know about the disease. Glaucoma is often detected at stage 2–3 or at the last, 4th stage, when it is often impossible to help a person. In Russia, glaucoma has recently become the first cause of irreversible blindness, overtaking injury and vascular eye disease. Despite a serious breakthrough in the understanding of many of the problems of glaucoma over the past few years, it must be admitted that so far no effective methods have been proposed to prevent the disease, its early (fairly cheap method!) Identification and treatment methods that are widely available. The trouble is that the prevention of this disease, we have long ceased. Previously, after forty, all Soviet people were sure to measure eye pressure once a year. In clinics there were professional examination rooms, people with elevated intraocular pressure were referred to an ophthalmologist. And so revealed about half of patients with glaucoma. Now there is nothing like this. Saving patients was the work of the patients themselves (that is, drowning people).  Since the treatment of glaucoma is just as dangerous as caving — you climb into the dark, and when and what falls on your head, science is unknown. But if you don’t fall, you will drown or suffocate yourself — there are options. When you guess where you are, it will be too late. Let me start with a number of rules described below. Rule number 1 If you have been diagnosed with glaucoma, this disease will accompany you throughout your life. This means that some part of the optic nerve has suffered. Therefore, one cannot say — “I have glaucoma removed” even after surgery. Living with glaucoma is not a sentence, but we must not forget about it. Rule number 2 This imposes a number of lifelong limitations and requires the regular use of drops — about them below. If you are respectful of your illness, the rate of its progression will slow down significantly. Rule number 3 Regular lifetime visits to an ophthalmologist are needed to monitor the level of intraocular pressure. Ideally, monthly. Once every 6 months you need to do research to assess the visual fields and tomograms of the optic nerves of both eyes. This is a dynamic control. Believe me, those patients who did not observe appointments lost sight, refused surgical treatment, disappeared for months and years, and then lamented that vision was irretrievably lost. Rule number 4 If nothing hurts, do not think that there is no disease and all the dangers are exaggerated. A feature of glaucoma is the absence of symptoms in the early and advanced stages of the disease. The patient himself does not know about the disease until he begins to lose his sight.  In order to notice the disease in time, preventive examination by an ophthalmologist is necessary. You need to pass it once a year, and after 50 years — twice a year. Rule number 5 Do not look for a “wonderful” pill, “magic” drops or devices that “heal all ailments”, which are so actively offered on the pages of newspapers, on radio and television, on the Internet, telling tips on how to cure glaucoma with folk remedies. This way you will lose that valuable time for treatment and it will be impossible to catch up. Use evidence-based medicine methods! What is the treatment for glaucoma currently? All types of treatment for glaucoma are aimed at normalizing intraocular pressure, improving nutrition in the tissues of the eye and in the optic nerve, as well as stabilizing visual functions. Conservative treatment of glaucoma That is, the instillation of various types of drops in a certain mode, and for each eye, it is selected separately. This therapy is most common in the early stages of glaucoma treatment. It can also be an addition to other types of treatment — laser or surgical. Some medicinal substances are aimed at reducing the production of intraocular fluid. Others, with the help of special mechanisms, are aimed at improving the outflow of intraocular fluid and thereby lowering the intraocular pressure. Also, there are combined drugs that combine both directions.  Are the drops of glaucoma harmless? Modern drops of glaucoma are in most cases effective, but not always harmless. Drops contain the active substance in the form of a solution, as well as a preservative, for example, benzalkonium hydrochloride. It has a negative effect on the eye surface. With prolonged use (we are talking about years), especially if the doctor does not change the drug, and the patient for a long time uses the same medicine, dry eye syndrome may develop (redness, pain, dryness). Allergic reactions and intolerance of drugs of the general and local character are possible. In addition, reactions of the body as a whole are possible, for example, interruptions in heart rhythm, lowering of blood pressure, sleep disturbance and dizziness, etc. A competent doctor from a huge arsenal of drops must choose a suitable one or find a replacement. If this does not work, surgical assistance is needed. Drug treatment of glaucoma is prescribed by an ophthalmologist only after a complete ophthalmologic examination is entirely individual — how it is written here. It is very dangerous to self-treat glaucoma — do not use or cancel antiglaucoma drugs yourself, do not violate the mode and frequency of instillation. With these actions, you can cause irreparable harm to your eyes and lose your sight.  And, here's another, in my (and not only) opinion — taufon and emoxipin, so loved by all — are useless with this diagnosis. Glaucoma and cataracts are not treated. The lens and the optic nerve do not reach. «Holy water» and more efficiently. Laser treatment for glaucoma 1. Patients love the word «laser.» So, only with angle-closure glaucoma, it is 100% effective. In cases of closed and narrow angles, a procedure such as laser iridectomy is the guarantor of prevention of an angle-closure glaucoma attack. In the case of angle-closure glaucoma (we wrote about it here ), the angle of the anterior chamber, in which the main outflow collector of the Schlemm's canal passes, is blocked by the iris root. By the way, this condition can be periodic, for example, it can manifest itself only when the pupil is dilated (at night, under stress, etc.). Predisposing factors — farsightedness (“short eye”) + “thick” lens (thickens with age) + front attachment of the lens + small front camera Then this is what happens:  The fluid accumulates in the back of the chamber, the iris overlaps the outflow channel, the pressure rises, the person experiences pain in the eye, the eye becomes red and there may be a loss of vision if you do not unlock the outflow. In this case, a hole is made in the iris using a perforator laser — peripheral laser iridectomy (iridotomy). It is also proposed to perform in the case when the angle of the front camera has not yet closed, but there is such a risk. Narrow angles are determined by inspection with a special goniscopic lens.  So schematically looks laser iridectomy and the eye after it under a microscope And here is a video of the procedure: Извините, данный ресурс не поддреживается. :( If the laser fails to perform the opening, surgical iridectomy is performed under operating conditions. Laser iridectomy is performed using laser systems with different wavelengths: using a single-pulse solid-state neodymium YAG laser or a gas argon laser. 2. Now about laser treatment for open-angle glaucoma. And I remind you that 80% of all cases it is she who is open-angle glaucoma. It's all not so simple. The varieties of laser surgery in the treatment of open-angle glaucoma are laser trabeculoplasty or trabeculo-puncture. The method involves applying point burn applications on a specific part of the trabeculae (the network through which the outflow is taking place).  It is assumed that the pigment that litters the trabeculae is “knocked out”, the fibers shrink and increase the spacing for outflow — they achieve a “popcorn effect”. For this, argon and neodymium laser trabeculoplasty (LTP) (514/532 nm) and diode infrared or micropulse LTP (810 nm) are used. In fact, such a procedure in itself can further increase the intraocular pressure, if the effect is, then it is very short-lived and unstable. As an independent procedure, it is dangerous, since after it the patients consider themselves to be a “cured” laser and often stop dropping drops and stop visits to the ophthalmologist. And glaucoma is quietly progressing! Laser procedures such as descemetonogonopuncture (BPH)With the help of these lasers, we often use in addition to microsurgical non-penetrating deep sclerectomy (NSEG), which will be discussed further. Then the shots are applied on the Descemet membrane, and not on the channel — it turns into a «sieve» and further enhances the outflow. 3. And finally, the laser for cyclophotocoagulation. In this case, it doesn't matter what was the cause. Used in the advanced end stage of the disease. When the eye does not see or hardly sees, it begins to hurt and bother. On the surface of the eyeball or from inside it (using an endoscope combined with a laser) coagulates are applied at a distance of 1.5 — 3 mm from the limbus in the projection area of the processes of the ciliary body, a rather painful procedure.  Outdoor cyclophotocoagulation (DPC)  Schematic representation of endoscopic cyclophotocoagulation. As a result of coagulation of the secreting ciliary epithelium, which produces intraocular fluid, intraocular pressure decreases. You can use a diode laser (810 nm) and neodymium laser (1064 nm). Therefore, the conclusion is that not all lasers are equally useful; a laser can eliminate the cause of glaucoma only with angle-closure glaucoma. A modern ophthalmologic clinic should have at least three types of laser systems for the treatment of various glaucoma variants. Surgical treatment of glaucoma Surgical treatment of glaucoma is aimed at creating an alternative system of intraocular fluid outflow, or at normalizing the circulation of intraocular fluid or reducing its production. This allows you to save the patient from drops or reduce dependence on them. The question of the surgical treatment of glaucoma is decided on the basis of the data of the dynamics of glaucoma strictly individually and depends on the form and its stage, the level of intraocular pressure increase, the outflow coefficient, the state of the anterior chamber angle, the visual field, and the general somatic state of the patient. Types of antiglaucoma operations 1. 1. Non-penetrating (non-fistulatizing) antiglaucoma operations. For example, non-penetrating deep sclerectomy (NSEG); In the upper part of the limbus, under the upper eyelid, a pocket of about 4 × 5 mm is formed in the middle layers of the sclera, part of the Schlemm's canal with its inner wall is exposed and removed, and the area of the Descemet membrane adjacent to the limbus is capable of filtering intraocular fluid. To extend the “service life” of this operation, drainage is placed in the pocket (it can be from different materials, for example, collagen) — this prevents adhesion of the pocket walls and scarring in the area of operation.  Usually this type of surgery is the primary choice for open-angle glaucoma, because:
 Outpatient microsurgery of glaucoma 2. 2. Penetrating (fistulizing) antiglaucoma operations. For example, trabeculectomy; In this case, a pocket is also formed in the middle layers of the sclera, part of the Schlemm's canal is removed, the eye is opened and the hole in the iris is surgically performed (the iris coloboma). The difference with the non-penetrating operation is in the opening of the eyeball — in the case of penetrating surgery, the eye is opened, in the case of non-penetrating surgery, a thin semi-permeable Descemet membrane remains intact, due to which the eye is sealed.  It is used in cases of more developed glaucoma and the need for a second operation. An older type of surgery, with various types of drainage that prevent scarring.  The patient's eye after surgery. Penetrating operations are more dangerous, as they can cause postoperative hypotension (long-term persistent pressure reduction), intraocular inflammation and hemorrhage, the appearance of cataracts, but have a longer service life. Types of drainage There are a great variety of drainage types — they differ in the type of material: hydrogel, collagen, metal and plastic. The shape can be rectangular, oval, square and triangular. They can be solid or porous, be a tube or a “nail.” There are so-called valve drains (Ahmed or Malteno) — this is a system of tubes with a plastic “pocket” that provide communication between the anterior chamber of the eye and the space between the eye shells. outflow. Inside the tubes are valves that are able to regulate the flow of intraocular fluid. Which is better? There is no ideal, everything is very individual. Everything as always depends on the experience and common sense of the surgeon. Ahmed’s valve looks like this schematically:  And so — «live»: 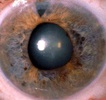 «Nail» -mini shunt, made of steel:  Drainage of gold is rather expensive and very fragile:  3. Operations that normalize the circulation of aqueous humor. For example, iridectomy (with closed anterior chamber angle).  In case the angle of the anterior chamber is blocked by the iris root, by opening the anterior chamber of the eye we can make a hole in the iris and restore the flow of fluid from the posterior chamber to the anterior chamber of the eye. Microsurgical techniques have made iridectomy less traumatic and practically safe operation. These operations include iridocycloretraction and others. This type of operation is less predictable in terms of efficiency, is associated with complications such as hemorrhages into the eye cavity, the appearance and rapid maturation of cataracts, and chronic inflammatory process. 4. Operations that reduce the production of aqueous humor. For example, cyclic cryoagulation. Cyclotriocoagulation is carried out at the terminal stage of glaucoma, as well as in the case of ineffectiveness of trabeculectomy or other similar operations. The zone that produces intraocular fluid can not only be destroyed by a laser — it can be “frozen”. During cyclocryocoagulation using a special cryoprobe on the surface of the sclera cause burns in the projection of the ciliary body, which are arranged in a circle. In the area of burns of a cryoprobe, cells of the ciliary body atrophy due to the influence of low temperatures. As a result, the amount of watery moisture produced is reduced. Exposure 1-2 minutes, 6-8 objects, temperature -130 ° — 150 ° C.  In short, a burn or frostbite helps to reduce pressure as an attempt to save the eye as an organ that, unfortunately, does not see. 5. Canaloplasty — plastic of the Schlemm’s canal. The canal of Schlemm (named after the German anatomist Friedrich Schlemm in the 9th-9th century) is the main transport collector draining aqueous humor (speed of about 2-3 microliters per minute) from the anterior chamber of the eye through numerous grids veins of the skull. This is a vessel that goes around the junction of the cornea and the iris in the thickness of the sclera in the corner of the anterior chamber. The channel in its structure resembles a lymphatic vessel. The inner part of the canal, which comes into close contact with the watery moisture, is covered with a microporous (trabecular) network. This site has the greatest resistance to the outflow of aqueous humor. If the canal trunk or its mesh structure is blocked, glaucoma will develop. It occurs in atherosclerosis, diabetes, injury or infection of the eye. This is how Schlemm's channel looks in full face and profile:  ОThe operations on the canal include expanding it with various probes and cans, holding special threads “in a circle”, dissection (ab interno trabeculectomy) and, finally, simply filling it with viscous fluids (for example, vysokanalostomy). It looks like canaloplasty thread:  However, such operations at best give a very short-lived effect due to scarring and recurrent blockage. But scientific research in this direction is constantly being conducted. When does glaucoma need surgery? Surgical treatment is an alternative to drug therapy in the initial stage and the only possible way to preserve vision and stabilize the disease in the advanced and advanced stages. Usually, a surgical operation for glaucoma is prescribed with a decrease or absence of the effectiveness of treatment with drugs and the loss of the effect of laser surgery for glaucoma. The period of rehabilitation after operations for glaucoma is usually minimal, there are some small limitations in the postoperative period, but the patient can start work after a few days. What is acute glaucoma? This is a very dangerous critical condition resulting from a sharp increase in intraocular pressure. An acute attack of glaucoma usually begins suddenly. Usually, with the appearance of pain in the eyeball, and the corresponding half of the head, especially often in the occipital region, it may be accompanied by nausea, often vomiting and general weakness. An acute attack of glaucoma can be confused with a migraine, hypertensive crisis, and even food poisoning; pains can spread to the area of the heart and abdomen that are similar to those in cardiovascular diseases. An acute attack of glaucoma appears for no apparent reason against the background of complete health — suddenly there are pains in the eye and in the head, the eye becomes red and watery, the vision decreases, there may appear “rainbow rings” around the sources of light and fogging. The intraocular pressure may increase to 60–80 mm Hg. Art., stops almost or completely outflow of intraocular fluid from the eye. To the touch such an eye becomes as dense as a stone. Errors in the diagnosis are expensive, as the patient begins to be treated for another condition, and the necessary emergency care in case of an acute attack does not have glaucoma. If, within 1-2 days after the onset of an attack, the intraocular pressure is not reduced with the help of drugs, laser or surgically, the optic nerve dies and the loss of vision becomes irreversible.  Other posts on the topic
=========== Источник: habr.com =========== =========== Автор оригинала: Tatiana Shilova ===========Похожие новости:
Блог компании Клиника офтальмологии доктора Шиловой ), #_biotehnologii ( Биотехнологии ), #_zdorove ( Здоровье ) |
|
Вы не можете начинать темы
Вы не можете отвечать на сообщения
Вы не можете редактировать свои сообщения
Вы не можете удалять свои сообщения
Вы не можете голосовать в опросах
Вы не можете прикреплять файлы к сообщениям
Вы не можете скачивать файлы
Вы не можете отвечать на сообщения
Вы не можете редактировать свои сообщения
Вы не можете удалять свои сообщения
Вы не можете голосовать в опросах
Вы не можете прикреплять файлы к сообщениям
Вы не можете скачивать файлы
Текущее время: 14-Янв 22:39
Часовой пояс: UTC + 5
