[Биотехнологии, Здоровье] Retinal detachment — what is important to know about it (перевод)
Автор
Сообщение
news_bot ®
Стаж: 7 лет 11 месяцев
Сообщений: 27286
Retinal detachment is a formidable eye disease that, without surgical treatment, most often results in complete loss of vision.
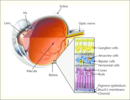
The human eye can be compared with the device of the camera, the lens of which is the cornea with the lens, and the film is the retina, an extremely complex multi-layer structure that is connected to the visual divisions of the brain with the help of nerve fibers. Therefore, we can assume that the retina is a part of the brain.
Retinal detachment most often takes the patient by surprise — before it appears, a person may have excellent vision and may not present any complaints. The speed of propagation of the process is quite rapid, the treatment in the majority of cases is surgical.

The timeliness of the operation gives a chance to preserve vision; in Germany, according to the standard, the operation must be performed within 24 hours after the diagnosis. There are no such standards in Russia. But for each patient, I say that retinal detachment is “like fresh frozen fish” — in a couple of days it’s already “not the first freshness”.
There are many methods of treatment for retinal detachment, they differ in the mechanism of action, they can be combined with each other, there are no better or worse ones among them — all are very individual.
Prevention (but not immunity) for retinal detachment exists — it is laser coagulation of areas on the retina, which may be the cause. These are certain types of dystrophies, tractions, breaks — but, unfortunately, not every patient believes in the need for these procedures, especially if nothing is bothering you.
CAUSES OF RETINA DISCONNECT
Detachment is the separation of rods and cones, we call them neuroepithelium, from the underlying pigment epithelium by the accumulation of fluid between them. This disrupts the power of the outer layers of the retina, which leads to rapid loss of vision.
The possibility of detachment due to the characteristics of the structure of the retina, I wrote about this in previous posts.
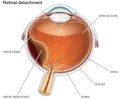
Retinal detachment in its type may be dystrophic (rhematogenous), traumatic and secondary. The secondary is not considered as an independent clinical form, but is only a complication of the underlying eye disease — inflammation, tumor, vascular or congenital diseases.
The reason for regmatogenous (regma — rupture) retinal detachment, or, they say, primary detachment, as is already clear, is a rupture or rupture of the retina. As a rule, the gap occurs somewhere on the periphery, close to the equator of the eye, in the area of thinning and dystrophy.
Types of dystrophies, dangerous in terms of delamination, have already been mentioned in posts earlier:
How to “sew up” the retina and should it be done?
The names of dystrophies are non-standard: “Lattice dystrophy”, “dystrophy by the type of snail track”, “traction”, “frivolous”, “white without impression”, “perforated breaks with and without lid”, “valve breaks” and others.

This is how dystrophic foci require coagulation (before and after the procedure).
PREVENTION OF RETINA DETACHMENT
From prophylaxis, the onset is intentional, because a timely preventive procedure can reduce the risk of exfoliation by an order of magnitude.
Since the previous posts described in detail how this happens, I want to draw attention to some points.
1. We say that, as a rule, laser coagulation is not a painful procedure, but there is always an amendment to individual sensitivity. In some cases, it can be painful, and in particularly sensitive ones it can even be very painful. The following factors play a role:
— coagulation volume and localization of zones,
— laser type and model,
— patient's fit and behavior during it,
— palpebral anatomy (“deep-set” eye, large nose, etc.)
— Experience a laser surgeon and the right choice of contact lenses.
Conclusion: if you have a high pain threshold, you are afraid or you are uncomfortable during the procedure — be sure to warn the doctor in advance or during it, with the help of drugs we can greatly facilitate the process of laser coagulation.
DIAGNOSTICS OF RETARDIUM DISEASES

The process of optical coherent tomography of the retina (OCT) in our clinic.
Diagnosis of retinal detachment involves primarily a complete ophthalmologic examination with eye examination, intraocular pressure, fundus examinations in various ways — contact and non-contact. You may also need to inspect both vertically and horizontally.
Special additional diagnostic methods are:
1. Perimetry. A frequent symptom of detachment is «veil» or «curtain» in front of the eye, it looks like this:

2. Ultrasound scanning in 2-D or 3-D mode. Allows you to define a detachment through the opaque optical medium of the eye or areas inaccessible to the examination… You can determine its height, the contents under it, the relief, the thickness of the shells — this is important.

3. Electrophysiology — as an eye cardiogram — captures electrical potentials from functioning areas of the retina, indicating the extent of its damage.
4. Optical coherent tomography — we obtain linear retinal sections to determine the anatomical parameters of the smallest sections in the central and close to it areas. The result may be a two- or three-dimensional image.

5. X-ray CT of the retina — provides visualization of the structures of the eye, down to the smallest details.
6. MRI — shows the degree of violation and makes it possible to create a three-dimensional image of the eye.
SYMPTOMS OF THE RETINA DETACHMENT
Comparing the eye with a camera in which there is a film, we can say that somewhere on the edge of the frame there appeared a scratch of the emulsion layer. Well, what of this, you say, because almost the entire frame and the most important thing — the center of the “composition” — is still visible well. It turns out that this is not true. Through the gap begins to penetrate the fluid, flowing under the retina and thereby peeling it from the underlying choroid. On film, it looks as if an emulsion layer starts to blister around the scratch and peel off from the substrate. A person at this moment sees a rather characteristic picture of a “gray curtain” at the edge of the visual field. Depending on the location of the gap, the “curtain” can either spread quickly (within several tens of hours), closing the entire field of view, or crawl more smoothly (for weeks)

Vision in the development of retinal detachment
Quite typical of fresh retinal detachment is a symptom of “morning improvement”, when a person in the morning (after a long inactive lying position) reveals a significant improvement (reduction of the curtain, its blanching and the ability to see through it). By lunchtime it gets worse again, and by evening it gets worse.
It is clear that if the gap is located in the upper parts of the eye, the fluid quickly goes down and the exfoliation passes rapidly. If the gap is located below, then the detachment slowly «crawls» up, and the progression will be slower. However, the adhesions between the retinal zones and scars will be more pronounced — the time for their formation will be more.
TREATMENT
Treatment is necessary, and only surgical, there is no other way out. No drops, ointments, tablets, injections, absorbable means do not help, but only take time, which allows the detachment to develop further and further. The sooner competent surgical treatment is carried out, the better results it gives and the more it is possible to restore sight. The goal of surgical treatment was formulated more than 100 years ago and is to close (block) the retinal break.
At the initial stage of the disease, there is usually no need to enter the eye, and surgery consists of a local external impression in the projection of the rupture. To do this, use special seals made of soft silicone, which press the area of the gap, thus blocking it.
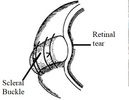
The scheme of episcleralisation
As soon as the opening in the retina closes, everything miraculously gets better, the “curtain” disappears, the vision begins to recover. Peripheral vision is restored first, the person discovers that the “review” is almost normal, and later on it really becomes normal. The periphery of the retina is fairly stable, and as soon as it becomes in its anatomical place, it immediately begins to “work” and recovers well even with long periods of retinal detachment. With central vision, things are not so simple. The most favorable cases are when the detachment did not have time to “crawl” to the center. For example, if the vision in the center remained 1.0, and the “curtain” closed the half of the field of view, after a successful operation, the vision could recover to 1.0, and the curtain would disappear.
If the detachment managed to close the central zone, after a successful operation, the central vision, unfortunately, can no longer fully recover. What will be the visual acuity after surgery in this case depends on a number of factors. The most important of them are the time during which the central zone of the retina has exfoliated, and the state of the blood supply to the retina, which directly depends on the age and degree of myopia (if there is one).
Restoration of central vision occurs slowly and usually almost ends at 3 months. Further improvement may continue, but at a still slower pace, and we observe that after a year, and after 3 years, visual acuity improves a little.

Changes in the structure of the retina after detachment, worsening the “picture”
If a person with retinal detachment is not operated on time or operated unsuccessfully, then the detachment remains and continues to develop, moreover, the so-called “proliferative process” begins in the vitreous.
The eye, as you know, has the shape of a sphere, and we already know that it has a lens, a retina film, besides this, inside the eye is filled with liquids. These fluids are almost 98-99% water, but with very substantial additives. The anterior part of the eye is bounded by the cornea on one side and the iris-lens block on the other. This part of the eye is more responsible for optics and is filled with anterior chamber intraocular fluid. In terms of its properties and appearance, it hardly differs from simple water with the addition of a complex set of minerals and salts.
Another thing is the fluid in the posterior part, bounded by the lens, ciliary body and retina. This liquid is called the vitreous body, it has the consistency and the appearance of a gel or frozen jelly. In addition, the basis of the vitreous body is a framework in the form of a voluminous lattice of collagen fibers.
When retinal detachment the vitreous body never remains indifferent. In the initial period, only small violations of its structure are observed, manifested in the form of various inclusions floating in the field of view. With a long-existing detachment in the framework of the vitreous body, strands develop, which, like ropes, attach to the retinal surface and, slowly contracting, retract the retina to the center of the eyeball. This process is called vitreoretinal proliferation, which ultimately leads to the formation of the so-called «funnel» retinal detachment. In such a situation, reconstructive surgery is required, in terms of the quality of a much higher level. Close this gap seals is almost impossible, and not enough. The main task is to clean the surface of the retina from the strands of the vitreous body, straightening it.
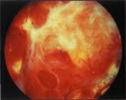
A picture of a severe form of proliferative retinopathy
For this purpose, special methods of so-called vitreoretinal surgery are used. Its essence lies in the fact that through point punctures with long and thin instruments the surgeon enters the eye and removes cords, freeing the retina and straightening it. The process itself is very similar to the painstaking work of the master, who collects a model of a XVIII century sailboat inside the bottle through the neck of the bottle with long tweezers and scissors.
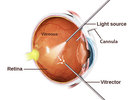
Vitrectomy (schematically)
This operation is very thin and complex, if you remember that the retina is extremely delicate and fragile nerve tissue, and almost every part of it is responsible for any part of the vision. During the operation, the doctor looks inside the eye through his anterior segment, peeks «through the pupil.» This requires a high transparency of the optical media, that is, the cornea lens and lens should be as transparent as possible. If the lens is cloudy, that is, the patient has a cataract, then, as a rule, at the initial stage, the lens is replaced with an artificial one, and only then proceed to «repair» the retina.
How we do this is discussed in these posts:
Cataract: it is waiting for you personally (if you live, of course)
We implant an artificial lens (you will need it after 60 years)
In addition, the natural lens, due to its anatomical location, often interferes with the work on the peripheral parts of the retina. In these cases, it is also necessary to change the lens to an artificial one, otherwise the untreated areas of the peripheral retina may not allow its anatomical fit to be achieved.
The operation is performed in the “dark room”, that is, only the light guide in the surgeon’s hand or the additional light source “chandelier” lights up the working field as a chandelier, the light of the microscope is turned off.

Outwardly, it happens like this (photo from the operating room)
After complete purification of the retinal surface from the vitreous cords, it must be straightened and placed on the choroid, that is, get its anatomically correct position inside the eye. For these purposes, the so-called “heavy water” is often used — liquid perfluororganic compound (PFOS). By its properties, this substance hardly differs from ordinary water, but due to its higher molecular weight it acts as a press on the surface of the retina, smoothing and pressing it. “Heavy water” copes very well with the detachment, in addition, it is absolutely transparent, and the eye filled with this liquid begins to see almost immediately. The main disadvantage is that the eye does not tolerate it for a long time. A maximum of a couple of weeks, but in practice for more than 7-10 days, it is undesirable to leave this liquid in the eye.
VIDEO VITRECTOMY SURGERY
Извините, данный ресурс не поддреживается. :(
Unfortunately, retinal glue has not yet been invented, but the laser turned out to be very effective. The laser “welds” the retina to the underlying tissues along the edges of all the breaks. After the application of laser coagulates, local inflammation occurs, and then a microtubule is gradually formed (5-7 days) on the choroid. Therefore, it makes sense to leave “heavy water” in the eye for a week. In some cases, this is enough to keep the retina in place, but it may be necessary to continue to hold the retina to form more durable adhesions. In such cases, silicone oil is used, which fill the eye cavity.

Variants of silicone oil of varying degrees of viscosity
Silicone is a clear, viscous liquid, the tissues almost do not react to it, so you can leave it in the eye for much longer. Silicone is not so good straightens and presses the retina, but to keep the retina unfolded, it fits perfectly.
The eye filled with silicone almost immediately begins to see, the retina retains its anatomical position, its functions are restored, and the adhesions in the areas of laser coagulates become very durable over time. One of the features of silicone is a change in the optical characteristics of the eye to the plus side by 4–5 diopters. Usually silicone is in the eye for about 2-3 months, after which the retina no longer needs any “props” and can be safely removed. This is also an operation, but not as complicated and voluminous as the previous ones.
In some cases, changes in the internal eye structures are so pronounced that the only option today is to have at least residual vision, or to keep the eye as an organ — is the constant presence of silicone in the eye cavity. In these cases, silicone can remain in the eye for many years, even decades.
In addition to «heavy water» or silicone oil, for the same purpose, various gases or air are sometimes used. Principle one, from the inside, press the retina for a while with the air bubble until the scars get stronger. Any gas, especially air, dissolves over time into the eye fluid and disappears. The air dissolves within 1-2 weeks, the gas can be in the eye for up to 2 months. Unlike silicone, a person with injected gas sees practically nothing except light and bright objects. Gradually, the boundary appears between the gas bubble and the ophthalmic fluid. The patient notes the fluctuations of the bubble when moving the head. As the gas is absorbed from above, the image begins to open and, eventually, the entire field of vision becomes clear. Thus, surgical treatment takes place in one stage — you do not need to remove air or gas.

This is how gas looks schematically, in the stage of resorption in the vitreous cavity.
All methods and substances used today in vitreal surgery are only tools for one big task — restoring vision after retinal detachment. Each case of detachment is individual and only the surgeon can decide what is best for a particular eye and for a particular patient. We can say with confidence that, using and combining modern methods, we manage to cope with almost any detachment. Another question is how damaged they are, how long the nerve cells of the retina did not work and to what extent they can recover after receiving its complete anatomical fit.
Summing up, we can say the following: all detachments, unsuccessfully operated on or for some reason not operated, can and should be tried to heal if no more than 1 year has passed since the moment of detachment and the eye sees the light with confidence. In these cases, there is a chance to achieve vision. If the eye does not see the light, then, as a rule, it is impossible to help. If the period of detachment is more than a year, the situation must be considered individually, sometimes it is possible to help in such cases.
How do the machines on which we operate on the back segment of the eye, and in what other cases, need a vitrectomy operation — removal of the vitreous body — in the next post.
===========
Источник:
habr.com
===========
===========
Автор оригинала: Tatiana Shilova
===========Похожие новости:
- [Искусственный интеллект, Машинное обучение] Как видит компьютер
- [Биотехнологии, Здоровье] Bionic eye — myths and reality (перевод)
- [Биотехнологии, Здоровье, Лазеры] How to “sew up” the retina and should it be done? (перевод)
- [Биотехнологии, Здоровье] Astigmatism — vision as in the kingdom of «crooked mirrors» (перевод)
- [Математика, Научно-популярное, Здоровье] Непростая математика коллективного иммунитета к коронавирусу (перевод)
- [Научно-популярное, Биотехнологии, Химия, Экология] Паучий шелк из фототрофных бактерий
- [Биотехнологии, Здоровье] Glaucoma — how not to go blind: let's talk about the treatment… (перевод)
- [Финансы в IT] Разбор: почему SoftBank планирует продать акции телеком-гиганта T-Mobile на $21 млрд
- [Биотехнологии, Здоровье] Glaucoma — not heard of it? Meet the serial silent view killer (перевод)
- [Здоровье] Как сбросить более 20 кг за несколько месяцев и не набрать их обратно
Теги для поиска: #_biotehnologii (Биотехнологии), #_zdorove (Здоровье), #_retinal_detachment, #_eyes, #_vision, #_eye_clinic, #_retina, #_blog_kompanii_klinika_oftalmologii_doktora_shilovoj (
Блог компании Клиника офтальмологии доктора Шиловой
), #_biotehnologii (
Биотехнологии
), #_zdorove (
Здоровье
)
Вы не можете начинать темы
Вы не можете отвечать на сообщения
Вы не можете редактировать свои сообщения
Вы не можете удалять свои сообщения
Вы не можете голосовать в опросах
Вы не можете прикреплять файлы к сообщениям
Вы не можете скачивать файлы
Текущее время: 14-Янв 22:39
Часовой пояс: UTC + 5
| Автор | Сообщение |
|---|---|
|
news_bot ®
Стаж: 7 лет 11 месяцев |
|
|
Retinal detachment is a formidable eye disease that, without surgical treatment, most often results in complete loss of vision. The human eye can be compared with the device of the camera, the lens of which is the cornea with the lens, and the film is the retina, an extremely complex multi-layer structure that is connected to the visual divisions of the brain with the help of nerve fibers. Therefore, we can assume that the retina is a part of the brain. Retinal detachment most often takes the patient by surprise — before it appears, a person may have excellent vision and may not present any complaints. The speed of propagation of the process is quite rapid, the treatment in the majority of cases is surgical.  The timeliness of the operation gives a chance to preserve vision; in Germany, according to the standard, the operation must be performed within 24 hours after the diagnosis. There are no such standards in Russia. But for each patient, I say that retinal detachment is “like fresh frozen fish” — in a couple of days it’s already “not the first freshness”. There are many methods of treatment for retinal detachment, they differ in the mechanism of action, they can be combined with each other, there are no better or worse ones among them — all are very individual. Prevention (but not immunity) for retinal detachment exists — it is laser coagulation of areas on the retina, which may be the cause. These are certain types of dystrophies, tractions, breaks — but, unfortunately, not every patient believes in the need for these procedures, especially if nothing is bothering you. CAUSES OF RETINA DISCONNECT Detachment is the separation of rods and cones, we call them neuroepithelium, from the underlying pigment epithelium by the accumulation of fluid between them. This disrupts the power of the outer layers of the retina, which leads to rapid loss of vision. The possibility of detachment due to the characteristics of the structure of the retina, I wrote about this in previous posts. 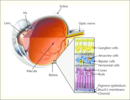 Retinal detachment in its type may be dystrophic (rhematogenous), traumatic and secondary. The secondary is not considered as an independent clinical form, but is only a complication of the underlying eye disease — inflammation, tumor, vascular or congenital diseases. The reason for regmatogenous (regma — rupture) retinal detachment, or, they say, primary detachment, as is already clear, is a rupture or rupture of the retina. As a rule, the gap occurs somewhere on the periphery, close to the equator of the eye, in the area of thinning and dystrophy. 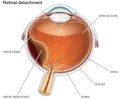 Types of dystrophies, dangerous in terms of delamination, have already been mentioned in posts earlier: How to “sew up” the retina and should it be done? The names of dystrophies are non-standard: “Lattice dystrophy”, “dystrophy by the type of snail track”, “traction”, “frivolous”, “white without impression”, “perforated breaks with and without lid”, “valve breaks” and others.  This is how dystrophic foci require coagulation (before and after the procedure). PREVENTION OF RETINA DETACHMENT From prophylaxis, the onset is intentional, because a timely preventive procedure can reduce the risk of exfoliation by an order of magnitude. Since the previous posts described in detail how this happens, I want to draw attention to some points. 1. We say that, as a rule, laser coagulation is not a painful procedure, but there is always an amendment to individual sensitivity. In some cases, it can be painful, and in particularly sensitive ones it can even be very painful. The following factors play a role: — coagulation volume and localization of zones, — laser type and model, — patient's fit and behavior during it, — palpebral anatomy (“deep-set” eye, large nose, etc.) — Experience a laser surgeon and the right choice of contact lenses. Conclusion: if you have a high pain threshold, you are afraid or you are uncomfortable during the procedure — be sure to warn the doctor in advance or during it, with the help of drugs we can greatly facilitate the process of laser coagulation. DIAGNOSTICS OF RETARDIUM DISEASES  The process of optical coherent tomography of the retina (OCT) in our clinic. Diagnosis of retinal detachment involves primarily a complete ophthalmologic examination with eye examination, intraocular pressure, fundus examinations in various ways — contact and non-contact. You may also need to inspect both vertically and horizontally. Special additional diagnostic methods are: 1. Perimetry. A frequent symptom of detachment is «veil» or «curtain» in front of the eye, it looks like this:  2. Ultrasound scanning in 2-D or 3-D mode. Allows you to define a detachment through the opaque optical medium of the eye or areas inaccessible to the examination… You can determine its height, the contents under it, the relief, the thickness of the shells — this is important.  3. Electrophysiology — as an eye cardiogram — captures electrical potentials from functioning areas of the retina, indicating the extent of its damage. 4. Optical coherent tomography — we obtain linear retinal sections to determine the anatomical parameters of the smallest sections in the central and close to it areas. The result may be a two- or three-dimensional image.  5. X-ray CT of the retina — provides visualization of the structures of the eye, down to the smallest details. 6. MRI — shows the degree of violation and makes it possible to create a three-dimensional image of the eye. SYMPTOMS OF THE RETINA DETACHMENT Comparing the eye with a camera in which there is a film, we can say that somewhere on the edge of the frame there appeared a scratch of the emulsion layer. Well, what of this, you say, because almost the entire frame and the most important thing — the center of the “composition” — is still visible well. It turns out that this is not true. Through the gap begins to penetrate the fluid, flowing under the retina and thereby peeling it from the underlying choroid. On film, it looks as if an emulsion layer starts to blister around the scratch and peel off from the substrate. A person at this moment sees a rather characteristic picture of a “gray curtain” at the edge of the visual field. Depending on the location of the gap, the “curtain” can either spread quickly (within several tens of hours), closing the entire field of view, or crawl more smoothly (for weeks)  Vision in the development of retinal detachment Quite typical of fresh retinal detachment is a symptom of “morning improvement”, when a person in the morning (after a long inactive lying position) reveals a significant improvement (reduction of the curtain, its blanching and the ability to see through it). By lunchtime it gets worse again, and by evening it gets worse. It is clear that if the gap is located in the upper parts of the eye, the fluid quickly goes down and the exfoliation passes rapidly. If the gap is located below, then the detachment slowly «crawls» up, and the progression will be slower. However, the adhesions between the retinal zones and scars will be more pronounced — the time for their formation will be more. TREATMENT Treatment is necessary, and only surgical, there is no other way out. No drops, ointments, tablets, injections, absorbable means do not help, but only take time, which allows the detachment to develop further and further. The sooner competent surgical treatment is carried out, the better results it gives and the more it is possible to restore sight. The goal of surgical treatment was formulated more than 100 years ago and is to close (block) the retinal break. At the initial stage of the disease, there is usually no need to enter the eye, and surgery consists of a local external impression in the projection of the rupture. To do this, use special seals made of soft silicone, which press the area of the gap, thus blocking it. 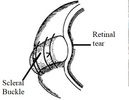 The scheme of episcleralisation As soon as the opening in the retina closes, everything miraculously gets better, the “curtain” disappears, the vision begins to recover. Peripheral vision is restored first, the person discovers that the “review” is almost normal, and later on it really becomes normal. The periphery of the retina is fairly stable, and as soon as it becomes in its anatomical place, it immediately begins to “work” and recovers well even with long periods of retinal detachment. With central vision, things are not so simple. The most favorable cases are when the detachment did not have time to “crawl” to the center. For example, if the vision in the center remained 1.0, and the “curtain” closed the half of the field of view, after a successful operation, the vision could recover to 1.0, and the curtain would disappear. If the detachment managed to close the central zone, after a successful operation, the central vision, unfortunately, can no longer fully recover. What will be the visual acuity after surgery in this case depends on a number of factors. The most important of them are the time during which the central zone of the retina has exfoliated, and the state of the blood supply to the retina, which directly depends on the age and degree of myopia (if there is one). Restoration of central vision occurs slowly and usually almost ends at 3 months. Further improvement may continue, but at a still slower pace, and we observe that after a year, and after 3 years, visual acuity improves a little.  Changes in the structure of the retina after detachment, worsening the “picture” If a person with retinal detachment is not operated on time or operated unsuccessfully, then the detachment remains and continues to develop, moreover, the so-called “proliferative process” begins in the vitreous. The eye, as you know, has the shape of a sphere, and we already know that it has a lens, a retina film, besides this, inside the eye is filled with liquids. These fluids are almost 98-99% water, but with very substantial additives. The anterior part of the eye is bounded by the cornea on one side and the iris-lens block on the other. This part of the eye is more responsible for optics and is filled with anterior chamber intraocular fluid. In terms of its properties and appearance, it hardly differs from simple water with the addition of a complex set of minerals and salts. Another thing is the fluid in the posterior part, bounded by the lens, ciliary body and retina. This liquid is called the vitreous body, it has the consistency and the appearance of a gel or frozen jelly. In addition, the basis of the vitreous body is a framework in the form of a voluminous lattice of collagen fibers. When retinal detachment the vitreous body never remains indifferent. In the initial period, only small violations of its structure are observed, manifested in the form of various inclusions floating in the field of view. With a long-existing detachment in the framework of the vitreous body, strands develop, which, like ropes, attach to the retinal surface and, slowly contracting, retract the retina to the center of the eyeball. This process is called vitreoretinal proliferation, which ultimately leads to the formation of the so-called «funnel» retinal detachment. In such a situation, reconstructive surgery is required, in terms of the quality of a much higher level. Close this gap seals is almost impossible, and not enough. The main task is to clean the surface of the retina from the strands of the vitreous body, straightening it. 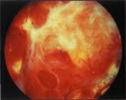 A picture of a severe form of proliferative retinopathy For this purpose, special methods of so-called vitreoretinal surgery are used. Its essence lies in the fact that through point punctures with long and thin instruments the surgeon enters the eye and removes cords, freeing the retina and straightening it. The process itself is very similar to the painstaking work of the master, who collects a model of a XVIII century sailboat inside the bottle through the neck of the bottle with long tweezers and scissors. 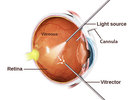 Vitrectomy (schematically) This operation is very thin and complex, if you remember that the retina is extremely delicate and fragile nerve tissue, and almost every part of it is responsible for any part of the vision. During the operation, the doctor looks inside the eye through his anterior segment, peeks «through the pupil.» This requires a high transparency of the optical media, that is, the cornea lens and lens should be as transparent as possible. If the lens is cloudy, that is, the patient has a cataract, then, as a rule, at the initial stage, the lens is replaced with an artificial one, and only then proceed to «repair» the retina. How we do this is discussed in these posts: Cataract: it is waiting for you personally (if you live, of course) We implant an artificial lens (you will need it after 60 years) In addition, the natural lens, due to its anatomical location, often interferes with the work on the peripheral parts of the retina. In these cases, it is also necessary to change the lens to an artificial one, otherwise the untreated areas of the peripheral retina may not allow its anatomical fit to be achieved. The operation is performed in the “dark room”, that is, only the light guide in the surgeon’s hand or the additional light source “chandelier” lights up the working field as a chandelier, the light of the microscope is turned off.  Outwardly, it happens like this (photo from the operating room) After complete purification of the retinal surface from the vitreous cords, it must be straightened and placed on the choroid, that is, get its anatomically correct position inside the eye. For these purposes, the so-called “heavy water” is often used — liquid perfluororganic compound (PFOS). By its properties, this substance hardly differs from ordinary water, but due to its higher molecular weight it acts as a press on the surface of the retina, smoothing and pressing it. “Heavy water” copes very well with the detachment, in addition, it is absolutely transparent, and the eye filled with this liquid begins to see almost immediately. The main disadvantage is that the eye does not tolerate it for a long time. A maximum of a couple of weeks, but in practice for more than 7-10 days, it is undesirable to leave this liquid in the eye. VIDEO VITRECTOMY SURGERY Извините, данный ресурс не поддреживается. :( Unfortunately, retinal glue has not yet been invented, but the laser turned out to be very effective. The laser “welds” the retina to the underlying tissues along the edges of all the breaks. After the application of laser coagulates, local inflammation occurs, and then a microtubule is gradually formed (5-7 days) on the choroid. Therefore, it makes sense to leave “heavy water” in the eye for a week. In some cases, this is enough to keep the retina in place, but it may be necessary to continue to hold the retina to form more durable adhesions. In such cases, silicone oil is used, which fill the eye cavity.  Variants of silicone oil of varying degrees of viscosity Silicone is a clear, viscous liquid, the tissues almost do not react to it, so you can leave it in the eye for much longer. Silicone is not so good straightens and presses the retina, but to keep the retina unfolded, it fits perfectly. The eye filled with silicone almost immediately begins to see, the retina retains its anatomical position, its functions are restored, and the adhesions in the areas of laser coagulates become very durable over time. One of the features of silicone is a change in the optical characteristics of the eye to the plus side by 4–5 diopters. Usually silicone is in the eye for about 2-3 months, after which the retina no longer needs any “props” and can be safely removed. This is also an operation, but not as complicated and voluminous as the previous ones. In some cases, changes in the internal eye structures are so pronounced that the only option today is to have at least residual vision, or to keep the eye as an organ — is the constant presence of silicone in the eye cavity. In these cases, silicone can remain in the eye for many years, even decades. In addition to «heavy water» or silicone oil, for the same purpose, various gases or air are sometimes used. Principle one, from the inside, press the retina for a while with the air bubble until the scars get stronger. Any gas, especially air, dissolves over time into the eye fluid and disappears. The air dissolves within 1-2 weeks, the gas can be in the eye for up to 2 months. Unlike silicone, a person with injected gas sees practically nothing except light and bright objects. Gradually, the boundary appears between the gas bubble and the ophthalmic fluid. The patient notes the fluctuations of the bubble when moving the head. As the gas is absorbed from above, the image begins to open and, eventually, the entire field of vision becomes clear. Thus, surgical treatment takes place in one stage — you do not need to remove air or gas.  This is how gas looks schematically, in the stage of resorption in the vitreous cavity. All methods and substances used today in vitreal surgery are only tools for one big task — restoring vision after retinal detachment. Each case of detachment is individual and only the surgeon can decide what is best for a particular eye and for a particular patient. We can say with confidence that, using and combining modern methods, we manage to cope with almost any detachment. Another question is how damaged they are, how long the nerve cells of the retina did not work and to what extent they can recover after receiving its complete anatomical fit. Summing up, we can say the following: all detachments, unsuccessfully operated on or for some reason not operated, can and should be tried to heal if no more than 1 year has passed since the moment of detachment and the eye sees the light with confidence. In these cases, there is a chance to achieve vision. If the eye does not see the light, then, as a rule, it is impossible to help. If the period of detachment is more than a year, the situation must be considered individually, sometimes it is possible to help in such cases. How do the machines on which we operate on the back segment of the eye, and in what other cases, need a vitrectomy operation — removal of the vitreous body — in the next post. =========== Источник: habr.com =========== =========== Автор оригинала: Tatiana Shilova ===========Похожие новости:
Блог компании Клиника офтальмологии доктора Шиловой ), #_biotehnologii ( Биотехнологии ), #_zdorove ( Здоровье ) |
|
Вы не можете начинать темы
Вы не можете отвечать на сообщения
Вы не можете редактировать свои сообщения
Вы не можете удалять свои сообщения
Вы не можете голосовать в опросах
Вы не можете прикреплять файлы к сообщениям
Вы не можете скачивать файлы
Вы не можете отвечать на сообщения
Вы не можете редактировать свои сообщения
Вы не можете удалять свои сообщения
Вы не можете голосовать в опросах
Вы не можете прикреплять файлы к сообщениям
Вы не можете скачивать файлы
Текущее время: 14-Янв 22:39
Часовой пояс: UTC + 5
